Philosopher Arthur Schopenhauer is famous for saying, “All truth passes through three stages: First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as being self-evident.”
As late as the 1950’s The Journal of Obstetrics Gynecology and Surgery had an editorial suggesting that all women should have a hysterectomy after their childbearing years. It seems the general consensus among doctors was that a woman’s reproductive organs are good for only one thing: childbearing, and after a woman has had all the children she wants, these organs are expendable, which then led to a worldwide push to perform these surgeries at an alarming rate. The highest rates are in the United States, followed by Canada and Australia.
Keep in mind, America became rich by developing the assembly line with the thinking that everyone benefits from the same treatment. But women are not identical and cannot be treated in this way. Of course, there are situations in which hysterectomy is required. But my question is always, why is this being recommended? And have other avenues of healing been explored? It’s a powerful question to behold, especially when it comes to your health and well being. My goal is always to empower you, dear reader, to make the very best decision with a team of providers that have your best interest at heart.
Today I’m joined again by Dr. Elizabeth Plourde, a clinical laboratory scientist and North American Menopause Society Certified Menopause Practitioner to talk about the dangers of hysterectomy and ovary removal.
In this episode, we discuss:
- Why women who have had their ovaries removed and do not take hormone replacement die younger with heart disease than women who take hormones
- The important role ovarian hormones play in keeping our tissues healthy and eliminating debilitating osteoporosis
- Why looking at root causes of excessive bleeding, fibroids, and cancer are the keys to healing
- Questions to ask your doctor if you are considering a hysterectomy
Listen to the episode here:
Within the below transcript, the bolded text is Samantha Gilbert and the regular text is Dr. Elizabeth Plourde.
___
The Truth About Hysterectomy and Ovary Removal
I realize today’s show may be a trigger for some of you, but the topic of reproductive health is just too important not to discuss, so I brought back Dr. Elizabeth Plourde, a clinical laboratory scientist and North American Menopause Society Certified Menopause Practitioner, to the show. In addition to being a practitioner and scientist who worked with hormone testing, and cutting edge cancer and DNA medical research laboratories, she spent over a decade researching women’s hormones, learning how women’s bodies function. From that research and those findings, she wrote Your Guide to Hysterectomy, Ovary Removal and Hormone Replacement, which explains how our ovarian hormones are critically important to maintain healthy tissues and women’s bodies.
20 years after her book was published, we now have studies published in 2021 and 2022 medical journals confirming her conclusions that our ovarian hormones are important throughout our lives and well past menopause. The studies confirm her findings that women who have had their ovaries removed and do not take hormone replacement die younger with heart disease than women who take hormones. Dr. Plourde’s book also reveals how ovarian hormones play important roles that keep our tissues healthy, so we do not die from osteoporosis, or suffer debilitating osteoarthritis. This book explains that the ovaries and uterus are not just for childbearing. They perform many functions and should be valued and preserved all throughout a woman’s life.
Elizabeth also consults worldwide assisting women to attain optimal hormone health, in addition to her career of research, consulting, teaching and writing. And through her own experience, she has become a passionate advocate, educating the public on sensible health practices. Elizabeth is also a hysterectomized woman, and the doctor that performed her surgery also took her ovaries and performed an additional procedure without her consent. Once she recovered, she dove into the research and found shocking data that revealed the truth of these procedures.
Today we talk about the importance of our vital organs and why these procedures are often more about making money than taking the time to address the root causes of excessive bleeding, fibroids, and other imbalances women face.
Thanks so much for being with us today. Here’s my conversation with Elizabeth.

Welcome back, Elizabeth. It’s great to see you today.
Thanks so much. I so appreciate being able to be back and to be able to share more information. So thank you.
My pleasure. Last time you were on the show, we talked about the harmful effects of sunscreen for which you’ve written two books. Today we’re going to talk about your experience as a hysterectomized woman, and your wonderful and very well researched book, Your Guide to Hysterectomy, Ovary Removal and Hormone Replacement, which is the culmination of 16 years of research. And I also want to make sure our listeners know that you are a North American Menopause Society Certified Menopause Practitioner. And while there have been some advances since you wrote this book, in my practice, I still see far too many women undergoing these procedures without true informed consent about the complications that can arise, as well as the importance of bioidentical hormone replacement post surgery.
So, Elizabeth, let’s start by going back in time, you wake up post surgery and everything is different. You’re in pain, confused, scared, and everything has changed. What was that like for you?
What Are the Dangers of a Hysterectomy?
Oh, it was, I actually was in disbelief, because the doctor had never talked about my ovaries, not once in any conversation, and I had been going to the doctors for three years asking for help, begging for help, trying to figure out what to do. Not one doctor, (I’d seen several doctors) not one mentioned, well, gee, we’ll take your ovaries at the same time as we take your uterus, which will solve your problem. And my problem was really a hormone imbalance. I didn’t have anything wrong with my uterus. And at the time, the OBGYN guidelines were to protect a woman, if she’s over 40, I was 43, to protect her from ovarian cancer sometime in the future, she should have her ovaries removed also.
And that was 35 years ago. And they have changed now. But at the time, there was nowhere to go because that was their policy. That was their guidelines. So today, they’re finally getting to the point that it’s amazing to see the articles, they start in 2021. Now a whole bunch in 2022, saying the ovaries are really important, and they should be protected. Women shouldn’t have their ovaries removed, it’s taken this long. My surgery was in 1985. It’s 2022. They’re finally recognizing the damage that loss of these organs creates.
I’m happy about that. I mean, there’s still a lot of work that needs to be done. I have to say in reading your book, which is so wonderfully written, not only the research aspect, because you’re an incredible researcher, but just how you personalize your story and really share your experience. It was so heartbreaking to read that the doctor took your ovaries and also cut the length of your vagina and resewed it tighter as some kind of favor to you. I mean, that just made me so angry for you. Like you said, he never mentioned that he would perform these additional procedures. You were not given any informed consent whatsoever. And when you asked him about this, he told you it’s just the normal thing we do. I just thought wow. I mean, that is insanity.
Yeah, it really is. And, you know, we decry the people from the Eastern countries coming over here and performing their clitoridectomies on their young women. And we think that’s so horrible, but there’s no difference. And ours has been heralded as normal medical procedures. And those are heralded as barbaric and trying to outlaw them and prevent them. But there’s no difference in what the woman is left with.
I’m so glad you made that correlation because it is the same. It’s barbaric. It’s inhumane, we just have this cloak of a clinical environment where “Oh, no big deal. It’s for your own good. Just be a good quiet little woman. Don’t worry about it. Don’t bother me.” I have to say, just reading that is shocking, absolutely shocking. I’m really curious, you mentioned hormone imbalance, which we’ll get into but why was this surgery recommended to begin with? What was your life like before the surgery?
I was in extreme adrenal fatigue. I was working an 80 hour a week job, being a single mother, and my ovaries were just overworked. And I wasn’t putting out enough progesterone to balance my estrogen. So I was bleeding horribly, to the point that I had to stay home with bath towels. That’s how badly I was bleeding. And this went on for three years as I consulted with different doctors. Not one of them mentioned progesterone. I wish that I had known about it at the time. Their only answer was hysterectomy. And I even sought out a female gynecologist thinking well, maybe she’ll know. And her answer was “it’s hysterectomy only.” So they didn’t really have the answers, the correct answers at the time.
I was so immersed in your book, I took so many notes. Again, I was shocked that you got this second opinion from a female gynecologist. And she said, “it’s your only avenue of relief, your life will be so much better afterwards.” Those were the two quotes in your book that really stood out to me. And also that, to your point, they didn’t even explore progesterone, they were only giving you estrogen. And when that didn’t work, they said, “Okay, now you need to have a hysterectomy.”
Right. And also they were giving me oral estrogen. And I did see my lab reports and my estrogen was zero. So the doctor already had the evidence in his hands that I didn’t absorb oral hormones. It was zero. So it was like he was giving me nothing. And so after they remove your ovaries, you really need estrogen. And he still only gave me oral estrogen, which didn’t do any good.
And we know the problems with oral estrogen now that they didn’t know back then I think, but did you have any recourse? You talked about in your book exploring, making a medical inquiry, correct?
Well, it was valueless. Because when you look at the OBGYN printed guidelines, it’s right in there to protect her from ovarian cancer. There’s absolutely no recourse, none.
Gotcha. Okay. So because the response from the medical board was they did everything right. Case closed, essentially. Is that correct?
Yes, that’s right. It was just common medical practice, which is one reason why I’ve written five books now about how the common practice is not very beneficial.
We’re so grateful for your books and you sharing your story. Going back to after you wake up from this surgery, and you’re in all this pain. And then the doctor says, “Oh, by the way, I did these other two procedures as well.” How did things progress from there? What was it like going through two years of hell and suffering before you got your life back? How did that impact your family, for example.
Why You Shouldn’t Get a Hysterectomy
Oh, my gosh, yeah, my daughter told me that she lost her mother, I was non-functional. I couldn’t work at all. And so I went from not working a couple of days a month during my period to not being able to work at all. I didn’t want to be out in public. I didn’t want to be around people. I just really hid in my bedroom. And we have a whole group of people that met at our house on Tuesday nights. And I just ran from the garage to my bedroom and stayed there all night.
Estrogen is a socializing hormone. That’s why we women are much more social than men. But losing it is just changing your whole life. I felt like I didn’t want to live anymore. It was just an incredible time. And I am very grateful. I was calling on doctors from Texas to Hawaii. So I went to all these OBGYN from all those states and asked for help. And the standard answer was, well, you’re mentally unbalanced. That’s why it’s called hysterectomy, to get rid of the hysteria in women, and you’re mourning the loss of your womb. That’s all that the problem is. And that was just ridiculous. I wasn’t mourning the loss of my womb. I almost died with my third child. And I was told to never get pregnant again. Why would I mourn the loss of a womb with that type of history?
Women shouldn’t have their ovaries removed. My surgery was in 1985. It’s 2022. They’re finally recognizing the damage that loss of these organs creates.
The thing is that when I was doing all my research at UCLA Biomedical Library, I found an incredible resource going back to the 1890s, of all the medical journals worldwide, and in 1895, women’s ovaries were being removed, which I can’t even imagine. To do that, I think they only had ether to help sedate the women. But those women were saying the exact same thing I said 100 some odd years later, exact same words of how they felt when they lost their ovaries. And they were told that they were mentally unstable prior.
Again, my heart breaks for what you experienced. And then I turn to anger because this is something I hear a lot in my practice in many of the women that I work with. Correct me if I’m wrong, but in your book you talk about how your pain was actually unchanged. And then there was this added severe depression and you were told you cannot be in pain, we removed everything. See a psychiatrist. I don’t even have any words for how that made you feel in that moment.
Exactly. That’s true. Yes, they don’t quite understand problems from your childhood that can cause pain in that area. When I’ve helped women who say they got their hysterectomy, they told the doctor, just get it out, I just want it out of my body, which can be from a lot of problems growing up as kids. The problem is not recognizing psychological trauma.
Yes, absolutely. I think we always need to look at history. I have a whole section on my intake form, just inquiring: Have you had any trauma or abuse in your life? I would say that most people have, if you’re listening to the show, and you have not, that makes me very happy. But most of us are going to experience some type of abuse or trauma in our lives. And how that affects us, physically, I think is really imperative to look at. And when you go through something like this, and trust is broken with medical professionals, that’s something else I see in my clinic where trust is so broken. And I often have to start very, very slow. And just slowly gain that trust and understanding that, “hey, I’m here to support you. I’m here to listen, I’m not here to talk down to you and tell you that it’s all in your head, because it’s not.” Everything that you’re experiencing is there for a reason.
And I always want women to know their discernment, and their intuition is important. It’s important to listen to that no matter what you’re being told, whether it’s from a doctor or a spouse, or another close loved one, I still encourage sticking to that and listening to that discernment. That intuition is there for a reason. So I’m so glad you shared that with us, walked us through what you went through. Just being able to recognize and see through your eyes, your experience, I think that’s important for what we’re about to talk about.
So, Elizabeth, after you got your life back, you dove into the medical literature and found out some pretty interesting facts that were not disclosed to you beforehand. I’d love to talk about and have you speak into what you found. What are some common misconceptions?
Common Misconceptions About Hysterectomy and Ovary Removal
Well, the thing that got me was that I realized that there was only one doctor from Texas to Hawaii who understood that I was experiencing loss of estrogen as well as loss of testosterone from my ovaries. And when there was only one doctor who understood, I thought, well, I’m only 43, I have a long way to go, hopefully, and that I need to figure out how to help myself. So luckily, I live near UCLA. So I literally lived in the UCLA library for 11 years in their Biomedical Library, reading everything I could, everything written worldwide, going back the 100 years that they’ve been doing these surgeries. I realized, as I was reading these articles, (I’m a clinical laboratory scientist with a biochemical foundation) that I could understand them.

The average woman without the scientific background would not be able to. So I made a vow to create a book to help women understand how their bodies work with their ovaries and do all the functions of the ovaries in all these hormones, so that they can make informed decisions because just removing women’s ovaries is not an informed decision, because they’re not being told. There’s over 1000 references in my book. So there’s no way a woman can not be informed with all the information that’s in these pages.
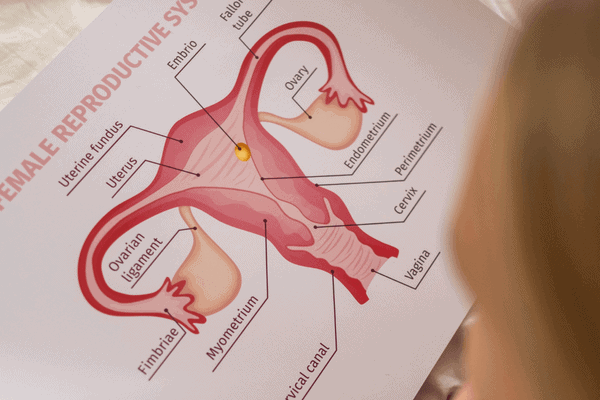
Good point. I appreciate you walking us through that. I think one of the things that was striking to me with all the research that you uncovered in your book, are the misconceptions. I’ll just list out here and we can talk about these: that the ovaries shut down at menopause, so no worries, you don’t need them anyway. They’re only needed for childbearing. Removing them reduces cancer risk. And then the other myth that really irritates me is that ovaries, if left intact, will continue to function optimally. And we know that’s not true. We know that when the uterus is removed, when the cervix is removed, problems will ensue because they all work together. They’re all connected. Our bodies are holistic for a reason. When I read that I was like, “Are you kidding?” I mean, it’s shocking to me that this was actually the common thought process of most doctors for many decades, correct?
The Ovaries Are Essential and Should Not Be Removed
Absolutely. For over 100 years. And it’s still, the doctors, the researchers who have recognized that the ovaries are essential and should not be removed, are decrying that, they’re still removing them because doctors haven’t gone to their continuing education classes to update their education. And so they’re still being removed today, without the recognition of how important they are. And I have the statistics in the book of the ovaries shutting down when the uterus is removed. And the doctors leave one ovary saying, “Oh, you’ll be fine with just one left over” but I’ve talked to enough men who have said that they lost one testicle and it was not the same. Both organs put out hormones, and we need that full supply.
Exactly. Yes, and going back to that first misconception, ovaries shut down at menopause. Well, we know the ovaries continue to produce hormones, even into menopause. So that’s a ridiculous notion. And just also think that, oh, they’re only needed for childbearing as if we’re only good for that, right? That’s beyond frustrating. And then decreasing cancer risk. We’ll talk about that in a bit because we know that’s also a myth. So I was fascinated by some of these numbers. In your book, you mentioned that 52% of hysterectomies caused women to lose their ovaries, and then it goes up to 76% between the ages of 45 and 55. And I also thought it was interesting that removal of the uterus alone will result in ovarian failure, which is going to lower things like FSH, bone density, progesterone, we talked about that a little bit.
I just want to reiterate, for our listeners that are maybe contemplating one of these surgeries, to see your body as a holistic organism, it works in synergy with every single part. And that’s why when you take one part, even if the ovaries are left, the level of hormones will decrease, I think exponentially and put you into early menopause. That was a really important aspect of our conversation that I really wanted to speak into. You mentioned the origin of the word hysterectomy a bit ago. Elizabeth, I’m curious, can we talk about that? Doesn’t that have a Greek origin like you said, hysteria? Interesting to use that terminology rather than to call it a uterectomy. Because that’s really what it is, correct?
Correct. That’s very correct, right. But that’s the myth of women and women’s psychology that perpetuated the whole surgery that if you take the uterus at least, maybe she won’t be so hysterical. It is just really sad because it really makes her more hysterical and depressed, hugely depressed.
Yes. And like you said, you don’t want to be around anyone. You don’t want to go anywhere. I’ve never had a hysterectomy. But I know what it feels like to struggle with severe depression and to be suicidal, and you had panic attacks. And I imagine that you had trouble sleeping as well, because sleep is a big part of this, too. I mean, was sleep, something that was severely impacted after your surgery?
It wasn’t so bad. But absolutely, these hormones are definitely connected to your ability to have nice deep, reparative sleep, and the serotonin the estrogen helps with. So it does, but it wasn’t a huge factor for me, as far as a problem.
That’s good. And you mentioned testosterone. And I think it would be fun to do a separate show just on testosterone, because many women and doctors included don’t realize how valuable testosterone is for us, even though we obviously make less than men do. It’s still a very, very important hormone for us.
It’s very important for our muscles. Very important. It’s very important for energy. So our normal values, I’m sorry to get into hormone replacement, but our normal values that are used in the lab, I was up at the maximum of women’s testosterone levels. And I had been there for quite a few years after my hysterectomy. And my sexual response had never really recovered from before the surgery and I just thought it was because I lost my uterus. And the uterus is very volved in sexual pleasure. I talked to a woman who had 12 fibroid tumors in her uterus and she said “the doctor never told me when he took out my uterus, that I would lose my sexual orgasm.” Because the uterus contracts during orgasm. And then all of those tumors gave her just this huge pleasure. Anyway, it’s part of the problem.
Yes, I appreciate you sharing that. Because my goal is always to educate and inform. And I think often women aren’t aware of what their anatomy is. So part of doing this show with you is to help educate women on anatomy. I’m trying to be more diligent, or making an effort to be more diligent with the term uterectomy, rather than hysterectomy. Because obviously, use of that terminology shows how little regard there is for women. I think it’s better now, but still needs a lot of work. But still, there’s this general disregard, I hear all the time, doctors telling women, “Oh, here, I’m just going to write you a script for an SSRI, oh, you’re just depressed, oh, just go see someone.” There’s still a lot of gaslighting that goes on. And it just makes me so angry. To be quite honest, I get so angry for the people that I serve.
So Elizabeth, you have an entire chapter on the ovaries, calling them finely tuned essential chemical manufacturing plants. I love it when you word it that way. So let’s talk about how a woman’s body deteriorates after these vital organs are removed, and she loses the natural protection of her hormones.
These hormones, there’s receptors for estrogen and essentially, almost every tissue in the body, our eyes, muscles, joints, even in our digestive tract, and in our intestines. They’re everywhere. There’s testosterone receptors in our digestive tract. And I have yet to find the research as to why we need testosterone in our digestive tract. But I’ve always thought that was interesting. But the estrogen receptors in our digestive tract are essential that they’re filled. We don’t absorb calcium unless there’s estrogen in those receptors. So we start losing bone immediately the day we lose our ovaries. We start losing bone, they can actually see it. And in a year, a woman is in full blown osteoporosis. It’s just amazing. The interaction.
There’s receptors for estrogen and essentially, almost every tissue in the body, our eyes, muscles, joints, even in our digestive tract, and in our intestines. They’re everywhere.
And one of the things that happened to me was I got horrendous, horrendous osteoarthritis, painful, painful, painful and I got fibromyalgia. The fibromyalgia had finally disappeared. I have a whole chapter on fibromyalgia in the book because it was so crippling to me during the time that I couldn’t get hormones I could absorb. I didn’t even want to get out of bed. And the doctor said, “Just go swim.” You don’t understand I can’t get this body out of bed, I was in that much pain. And when I found hormones I could absorb, in two weeks, the whole pain disappeared like a bubble burst, it was just gone. So we just don’t understand the complexity of our body and how it’s all interrelated.
The Ovaries: Finely Tuned Essential Chemical Manufacturing Plants
I’ve been having trouble ever since the FDA shut down compounding pharmacies from being able to make the hormones I absorb in their hormone pellet implants. And I started getting osteoarthritis again. And I finally found the pellets that I need. I have to go out of state because in California, they are robber barons and charging way too much for the pharmacy to try to get them in here. So I have to go out of state to get them implanted in my body. And all over the United States carry them with no problem, except California. I found them four months ago and got them implanted four months ago, and I just had them implanted again. One of the questions the doctor asked me was, “How’s your joint pain?” I had totally forgotten I had joint pain. When I saw him all my joints were hurting four months ago. But the four months on the hormone pellet implants, it just disappeared.
Sex Hormones Support Digestion, Blood Pressure, Cholesterol, and Bone Health
Wow. That’s amazing. I’m glad you spoke into digestion, because I often find that digestion becomes a big challenge after many of these surgeries. I’m glad you spoke into the fact that all of our sex hormones are connected to our digestive tract and receptors everywhere, especially in the digestive tract, and are needed for motility, needed for that whole process of digestion and assimilation. It’s critical and it’s amazing. I love bioidentical hormone therapy, it is very effective. But again, it’s not the same as what our body would make. And then also, we’ve got wonderful medical technology. But what about repairing damaged nerves that can happen during surgery or this beautiful patterning that occurs and the flow of hormones and chemicals when they’re naturally made that gets disrupted?
I’m glad you spoke into bone loss as well. Things like high blood pressure and cholesterol prolapse are also very common. Also, when the uterus has been removed, stroke, heart attack, weight gain, depression, anxiety, I mean, the list kind of goes on and on, bladder and bowel problems. It’s just fascinating how all of these downstream effects can occur so quickly, post surgery. Elizabeth, I don’t want to miss any aspect of focusing on the ovaries.
Yeah, they also make chemicals called prostaglandins. And those prostaglandins are critical for blood pressure, the uterus also makes them. So those chemicals are very important in maintaining normal blood pressure. One of the things that happened to me, I had been told my whole life that I would live to be 100, because my blood pressure was so good. 120 over 70 my whole life, and even in the ninth month of pregnancy, 120 over 70. And then the day after surgery, after they removed those organs, I was way high. Critically high. It was a horrible journey. I even had to go into the emergency room, my blood pressure was so high, and they wouldn’t let me leave until they gave me blood pressure meds.
There’s five groups of high blood pressure meds, I tried all five of them. Each one made me so sick in different ways that I finally decided I would rather have a stroke and die than to live like this. Then I finally found that CoQ10 regulated my blood pressure. But I have to take it. Before my surgery, I didn’t have to take CoQ10 to keep my normal blood pressure. It’s so amazing to me that Western medicine thinks they know so much that they can remove these organs and not understand the total impact on the total body. Because it is just astounding.
Estrogen: Our Natural Antidepressant
It is astounding. I think along the lines of high blood pressure, and then of course I mentioned cholesterol a bit ago and how estrogen alters the ratio of fats in the blood. It helps with artery cleanup, and it helps prevent plaque buildup, and actually acts as an antioxidant. And so when that’s gone, we often see very high levels of cholesterol. And of course, statins aren’t the answer. They’re very damaging to the liver among other things. So it’s this cascade, and then the thyroid gets involved and you can develop insulin resistance and then that can impact cortisol which can impact sleep. Again, just this long list of downstream effects that women are not told about before the surgeries and then add to that mood dysregulation. When depression can be so intense that you know you don’t want to live anymore and you can’t sleep and your anxiety is so high. I mean we know that estrogen is a natural antidepressant, it’s just fascinating to me how wonderfully made our bodies are. I never tire of learning about the human body.
I agree. I became a clinical laboratory scientist because I’m so in awe of how our bodies were so beautifully made. And even all these years later, I interned 50 years ago, they’re still discovering things about how intricate and complex our bodies are. So it’s just amazing how it all works together.
The Cervix: A Massive Nerve Complex
Yes, absolutely. I’d like to talk about the cervix now, because that’s another important aspect of being a woman. And I’m curious, why should the cervix be preserved? And what is its function?
It’s very important, and they just automatically removed it. I have to say that all these years later, the women that I speak with are being told that they can keep their cervix if they want to. And when I had my surgery, it was not an option, they just automatically removed it. And so I’m hoping that maybe my book and my chapter on the cervix has kind of changed that because it’s a central nerve junction, it’s very connected to sexual response and sexual satisfaction, because there’s so many nerves there, but also to prevent prolapse, organ prolapse. You don’t want scar tissue there. And it’s a bacterial barricade. So it prevents infections. To say that it’s not important just makes no sense.

Women that have their cervix left intact, don’t they have fewer complications, if they have their uterus removed, such as blood loss and the ability to return to normal life? Is that correct, Elizabeth?
Absolutely. Well, it’s such a huge nerve complex. It’s connected to so many places in the body. It’s connected to the bladder or the rectum. It’s just everything. And so when you take out a hole, it’s like missing a piece of a puzzle. The puzzle never is quite the same. And it’s not as strong. If you take out a piece.
Yes, good analogy. It’s amazing to me that they thought that it was okay to take it out. I am happy to hear that the tide is shifting in that regard. I think we’re not completely there yet. There’s still so much work that needs to be done in terms of education. But things are shifting a little bit.
I’m really curious, what are some common reasons women are told they need to have these procedures? I mean, the one I think of the most is fibroid tumors. And then of course, we talked about reducing cancer risk. Can you speak into that a little bit more, Elizabeth?
Common Reasons for Hysterectomy: Heavy Bleeding, Reduced Cancer Risk, Fibroids
One of the major reasons is the bleeding, the heavy bleeding. And that’s happening more and more because electromagnetic radiation reduces progesterone in our bodies. And the progesterone is what stops the bleeding. The corpus luteum is pure progesterone. And it just keeps dissolving putting progesterone into the system. And once that runs out, and we no longer have progesterone, we start the menstrual cycle. And more and more women are having problems with bleeding. And when their progesterone is measured, they’re very low in progesterone today. And it really is electromagnetic radiation that’s causing that.
Yes, that’s another important topic. I’d like to bring you back on the show for that. You’ve written a book about EMFs, as well, correct? Copper toxicity is another reason for excessive bleeding.
Estrogen alters the ratio of fats in the blood. It helps with artery cleanup. It helps prevent plaque buildup and acts as an antioxidant. So when estrogen is gone, we often see very high levels of cholesterol.
Yes, I have. And that’s part of it. All these things, the electromagnetic radiation being brought out with no warnings about the impact on every cell of the body and in the surgeries, no warning about the impact. It’s just there’s so much that’s been done. Without truly informing there’s no true informed consent.
I have to add to that our food supply. There isn’t global informed consent about what they’re really utilizing on our crops. We’re pretty familiar with things like glyphosate and other chemicals that they’re utilizing. But there are a lot of other things going on behind the scenes that we don’t even know about. And that’s a big part of what I try to do in educating people about what food really is and what it isn’t and what’s in the food supply that’s really impacting our bodies in this way, especially women and the dysregulation of our hormones. We can’t blame this on just stress anymore or hysteria, right? We have to look at our environment. And we have to look at what has shifted and changed and stop blaming women, you know, that are suffering, stop blaming the patients that are suffering and seeking relief.
I just want to add to what you were just saying about the food, we just attended a medical conference about the problems that children are having. And it was three days of different doctors every hour, a different doctor. And everyone seemed to end with its lack of vitamin D, lack of vitamin C, it’s omega three fatty acids, it was all down to nutrition, on all of these things that these children are demonstrating. And I think a large part of it is that those vitamins are missing in our food supply now, on top of the pesticides. So we also publish a book by Dr. Stephanie Seneff about glyphosate. It’s all the things that she sees that are causing our problems. It’s not just glyphosate, it’s EMF, it’s vaccines. She lists them all and describes biochemically why they’re all impacting our health. Food is definitely important.
I’m glad you spoke into that, Elizabeth, because in my area of specialty, which is nutrient therapy, I see it all the time. I see the deficiencies, I see them run in families, I see them passed on. And yes, you’re correct the soil is where it’s at, right? If the soil is depleted, and deficient, as ours is, especially here in the United States, then we’ve got problems, because our food supply is going to be deficient as well. So very important. I’m so glad you shared that.
So Elizabeth, when is a hysterectomy appropriate? And when is it not?
Hysterectomy Does Not Eliminate Cancer Risk
Well, it’s a very difficult question to answer. So 10% of uterine removal is for cancer. 90% is for fibroids, or the bleeding, or something else. It’s not life threatening. And there are answers to all of that without removing the uterus. And even then, I’ve talked to people who got the diagnosis of cancer and used other routes, determined to cure themselves, and they have. They’ve gone to different sources to help reduce the cancer, and they’ve been able to do so. And the same with the ovaries. The ovaries only 5% are for cancer, and the rest are all prophylactic to protect the woman from ovarian cancer. And it doesn’t even do that because the tissue is left in the abdominal cavity. And that can still turn cancerous. So the doctors aren’t even looking for it because they don’t have the ovaries. But it’s still a cancerous tumor.
Those numbers are staggering. To hear that, I didn’t realize it was that low.
Yes, it’s been used as a catch all. And it really shouldn’t be. These organs are too important. But you know, the value of women has been gradually increasing over the last couple 100 years. And hopefully it will continue with the latest research studies of 2022 saying that these organs are valuable, we need to preserve them. And hopefully that will start becoming the standard conversation rather than where we’ve been for over 100 years.
Yes, well said. And that kind of leads me into my next question. I still see there’s a trend to perform these surgeries on young women because cancer runs in their family, not because they actually have cancer. Of course, you and I are not fans of this. And like we were discussing, there are always underlying factors such as methylation, copper overload, and other deficiencies and so forth that can be corrected without the use of these invasive procedures. So what are your thoughts about this? Have you seen this in your own clinical practice? You mentioned some of the data about actual risk. But do you see this often?
The women who find me it’s usually after the fact, after the surgery. So it’s a little too late for that. And so then I try to help them get hormones that their body absorbs that they can finally feel like themselves again. I haven’t seen that.
The cervix is a central nerve junction. It’s very connected to sexual response and sexual satisfaction, because there’s so many nerves there, but also to prevent prolapse, organ prolapse. You don’t want scar tissue there. And it’s a bacterial barricade. So it prevents infections.
I would say I’ve not seen a lot of it in my practice. But going back to this, this notion of removal decreases the risk of cancer. You know, surgery doesn’t guarantee you’re not going to get cancer. I mean, I think we just need to be honest about that right now. We already talked about the importance of the ovaries and then of the cervix. And then of course, there are lifestyle factors that are going to influence risk. But I wanted to just touch on it briefly because it is something that I do see. It’s startling a young woman being told or dare I say almost coerced a little bit or pushed into how this would be best for her. Because you may get this in the future because this does run in your family. Well, guess what? Nutrient deficiencies and overloads run the family all the time, right? Crappy diets being passed on from generation to generation, because that’s just how you do it and families. But you can stop that cycle, you have that power, you really have a lot of choice in that regard.
Estrogen Loss Leads to Glaucoma
As far as that I’ve been suffering from glaucoma. And the ophthalmologist who’s been helping me, she had a patient go blind, because that’s what happens with glaucoma. And so she’s just hyper vigilant to stay on me. And I finally found out that it’s 17 beta estradiol that protects the eyes from glaucoma. And I’ve been suffering with, you know, not optimal levels for 35 years. And so it makes sense I have glaucoma. Well, when I first saw the doctor, I was asked, “Well, anybody in your family?” and I said, “My mother had glaucoma.” And his response was, “Well, yes. So that’s why you have it.” But my mother also had a hysterectomy. There you go. So it’s just amazing what 17 beta estradiol does in the eye, protecting it from glaucoma. Amazing.
Yes, I find all of them, when you look at all of them together, and how they work in harmony with one another, I’m always so fascinated and blown away by the human body, especially the female human body, and our ability to give birth and to carry a child for nine months and create a new life and bring that life into the world. It’s funny, whenever I watch a show where a child is being born, it makes me so emotional. I don’t know if you ever get emotional, maybe it’s just me. But there’s a show that I love called Call the Midwife. Oh, wow, I love that show. It’s a British show. It was a time back in the 50s and the 60s, when you actually had midwives that would go from home to home and help women give birth. And this is in London, and it’s just such a good show. And so every show, you’re watching these little babies be born and they make it look so real. It’s just fascinating to watch.
So, Elizabeth, I’m curious, what are some questions women should be asking before embarking on these procedures?
Hysterectomy Side Effects and Questions to Ask Your Doctor Prior to Surgery
Oh, golly, it is critically important to ask, “Will this really solve the problem?” Because lots of times, it can solve that problem, but it’s creating so many more. I think that to understand the complexity of our body, we need these organs in there. When you cut the uterine ligaments, they’re the strongest in the body, they have to be in order to support the nine month fetus, then the back starts falling down. So women start having problems because their backs no longer stay stable, the vertebrae start falling down. And that’s a huge problem. It really is tremendous. I still suffer with that today, I have to really work on my muscles to keep my muscles strong, to keep my back in alignment. And you’re never warned of that either.

Just to add on to that Elizabeth, what about additional surgeries that might be required to repair some of these things to repair the bowel, to repair the bladder. IBS is also a problem with a lot of these procedures, bladder and urinary tract infections. I think about all of those things that aren’t disclosed. And then what about the mortality rates? Can we talk about that a little bit, because that’s in your book as well
Yeah, I’m not sure if it’s changed. I mean, because the book is about 20 years old now. So I haven’t looked up statistically but women do die in surgery. All surgery has a death associated with it at some time. It’s really important to realize that maybe this quick short answer that they’re saying will solve all your problems could result in your death. I can’t really remember what the statistics were but I don’t know what they are now, but they probably don’t change because surgery is a set mortality rate on all of them.
Yes, good point, and you know, things get normalized. And so we don’t think of mortality. But this is major surgery, major surgery, and you’re taking something out of your body, that is a huge part of who you are, as a woman. I didn’t want to forget to mention that I agree with you. We don’t know the actual stats, that’s okay. But it is something to consider. So if you are listening to the show, and you’re being told that you need to have one of these procedures, I want you to make a list of these things that you should be asking, for example, hormone replacement is going to be a must, ask about mortality, ask about damage during surgery to your nerves and blood vessels. Ask about additional surgeries that may be needed to have bowel repair or bladder repair.
And I think in your book, I recall reading this Elizabeth that 59% of women and again, we don’t know what the stats are now, unless you do, but 59% of women report worsening symptoms or even new symptoms, because you’re taking away so much post surgery. That’s significant. 59% I’m like holy cow, that’s a lot.
Hysterectomy and Bladder Incontinence
One of the things is bladder incontinence. I just shudder when I go down the Depends aisle at the grocery store. Because all women need is to not have surgeries. And then also proper hormone replacement. And proper hormone replacement is not happening. The FDA is not our friend in that. And I am so grateful that I finally found hormones that are manufactured the way I need them for my body. And I can feel my body gradually getting better. But I want to warn our women that laboratory tests do not tell you the truth about where your hormones are.
I had to have one of my doctors tell me, you need more testosterone when I was already at the top of women’s replacement, and doctors are not going to give it to you if you’re already at the top. But I luckily had a doctor who understood that I obviously made more testosterone than the average woman my whole life. When I did testing in college about what I wanted to do, I got D’s and F’s on all the women’s, the whole women’s test D’s and F’s. And so luckily, the counselor said, well, let’s give you the men’s interest and I got A’s all across the top because I make more testosterone and I have a more masculine way of looking at the world. I also needed to replace more testosterone than the average woman would need to.
And I’m so glad you spoke into that. I’m also glad that you were able to find someone because what the FDA has been doing with regard to bioidenticals and compounding and especially with testosterone, there hasn’t been a lot in the mainstream news, of course, because they won’t cover it. But within the holistic community and the functional community, it’s been something that we’ve been talking about for quite some time. And I’m just so sorry that you have to jump through so many hoops just to get hormones so that you can feel like a woman and live your life and be healthy and enjoy life and all that goes with that. I mean, it’s just ridiculous. I say this all the time because it’s so true. We have to work so hard to be healthy because the system wants us to be ill. Isn’t that sad?
It really is. There’s also so much ignorance as to what health is. I don’t know if it’s because they want us to be ill. They are ignorant of how we aren’t healthy. That’s part of the problem and the hormone replacement therapy is just tragic because every single woman absorbs differently. Every single woman’s requirements are different. And I go by symptoms when I’m working with women, rather than the lab tests because I so mistrust the lab tests, but doctors don’t work with symptoms, and they used to before the laboratory tests.
I finally found out that it’s 17 beta estradiol that protects the eyes from glaucoma.
I’m very grateful for the family doctor in 1958 when I was 15. The family doctor prescribed thyroid for me, due to my symptoms, and the laboratory tests for thyroid didn’t come out till the 1970’s and I test normal on the thyroid tests, they don’t work with the genetically inherited low thyroid I have, because it’s not the value in the bloodstream. It’s that we have mitochondria that can’t utilize the thyroid hormone. So if the thyroid tests were out before the doctor diagnosed me, he would have done the test and said, “Oh, you’re normal” and then went on to something else. But I absolutely need thyroid. And I’ve been using it since I was 15.
I think it’s important to note that no test is 100% accurate. Absolutely. I tell that to the people that I work with all the time. I do utilize testing in my clinic, it is a helpful tool. But I agree, we also have to look at symptoms, we have to get to know our clients and our patients on that deep level, we must listen to show empathy and compassion. Obviously, the training that goes along with that is really imperative. I’m glad you spoke into that and the importance of being able to look at symptoms and health history and family history and all of those markers. I know I have similar stories, myself. And there are thyroid challenges and different types of imbalances and nutrient deficiencies that run in my family as well. And it’s been quite a journey for me over the last 20 years, but I’ve had my practice for a little over 13. And it’s been an amazing journey. And you know, we’re always learning as practitioners, we’re always researching and studying. And like you said, there’s still things that we’re uncovering and figuring out and I think that’s the beauty of this work and just helping people be whole and happy.
I want to share with you that I’ve been doing menopause consulting, for over 20 years, around the world. And I can’t tell you the number of women who call me desperate, absolutely desperate, with a huge amount of symptoms. And saying my doctor tested my blood and he says all my hormones are in normal range, so he won’t give me any hormones. So then when I have them fill out my six page profile, that’s mostly symptoms, and as I’m reading it, I hurt. I know how bad they feel, it just hurts inside for them. Because they obviously need the hormones and the hormone tests are just not valid at that point. It’s just really sad.
Yes, it is sad. How can women contact you for consultations?
They can email on our website. We’ve had so much trouble with our website, we’re still recovering from all the hacking that went on with our website.
Okay, wonderful. Thank you, Elizabeth. Any last words for our listeners, anything else you’d like to share?
Don’t trust the medical field.
Well said.
It staggers me. You know, they’re so wrong. And so many points are so wrong on gallbladder removal. They’re so wrong about cholesterol. Normal cholesterol values 50 years ago were 240 to 280. That is our normal cholesterol. Because all of our hormones are made from cholesterol, we need cholesterol to make our hormones. And they want it to be 200 and below, it’s absurd. And I’ve done hormone lectures and had men come to me afterwards and say, I’m on statin drugs. Could that be why I can no longer perform in the bedroom? Because they’re not making testosterone to be able to have their sex drive.
Yes, I’ve seen that too. That’s a whole other show as well. Yes, statins and cholesterol.
The medical community is so far off. And the problem is how do you find the answers? The right answers, because they’re really getting more difficult to get on the internet.
Yes, that is correct. Good point. Wonderful. Well, thank you so much, Elizabeth. Thank you for your knowledge and your wisdom. And we’re just so glad to have you and all the books that you’ve written that have helped so many people.
Thank you. Oh, thank you for helping spread the word and for what you’re doing because it’s getting the word out that people can be helped. So thank you.
Thank you so much for being part of this important conversation. I’m very grateful to Elizabeth for dedicating her life’s work to shining a light on the truth about these procedures and how women can be their own best advocates. Elizabeth reminds us that everyone needs to become their own health advocate, starting with researching what is truly healthy for our bodies, and always asking questions of our medical providers.
Important Links:
- Elizabeth’s book: Your Guide to Hysterectomy, Ovary Removal, & Hormone Replacement: What All Women Need to Know
- Elizabeth’s Website
- Premature or Early Bilateral Oophorectomy: A 2021 Update
- Physician attitudes and knowledge on prophylactic salpingectomy in perimenopausal patients
- Associations between menopause, cardiac remodeling, and diastolic function: the CARDIA study
- Risk of de novo severe carpal tunnel syndrome after bilateral oophorectomy: a population-based cohort study
- Learn more about copper toxicity