Autoimmune diseases have become increasingly recognized in recent years, but they remain a complex and often misunderstood area of health. Understanding autoimmune diseases is crucial for those who suspect they may be affected, as well as for healthcare professionals aiming to offer the best care. In this comprehensive guide, we will delve into what autoimmune diseases are, their causes, common types, symptoms, diagnosis, and treatment options.
What Are Autoimmune Diseases?
Autoimmune diseases occur when the immune system, which is designed to protect the body from harmful pathogens, mistakenly targets and attacks its own tissues. This malfunctioning immune response leads to inflammation and damage to various organs and tissues. The exact cause of this misguided immune reaction involves a complex interplay of genetic, infectious, environmental, and hormonal factors.
Common Types of Autoimmune Diseases
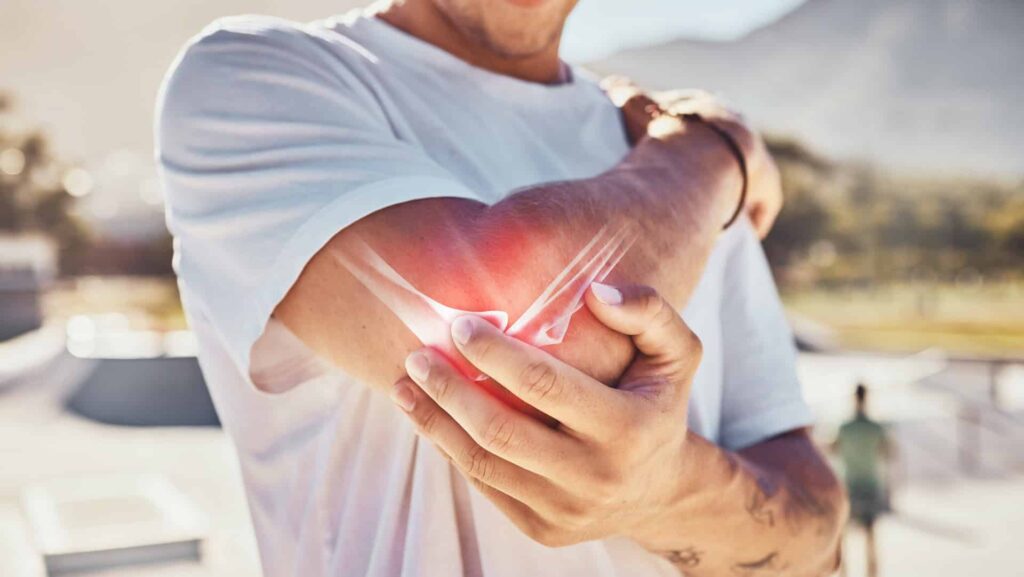
Rheumatoid Arthritis (RA)
This disease primarily affects the joints, causing pain, swelling, and stiffness. Over time, RA can lead to joint damage and deformity.
Systemic Lupus Erythematosus (SLE)
Lupus is a systemic autoimmune condition that can affect multiple organs, including the skin, kidneys, and heart. Periods of flare-ups and remissions are what identify it.
Multiple Sclerosis (MS)
MS involves the immune system attacking the protective covering of nerve fibers in the central nervous system, leading to various neurological symptoms such as numbness, difficulty walking, and vision problems.
Type 1 Diabetes
In this condition, the immune system attacks insulin-producing cells in the pancreas, leading to high blood sugar levels and requiring lifelong insulin therapy.
Hashimoto’s Thyroiditis
This autoimmune disorder affects the thyroid gland, leading to hypothyroidism, characterized by symptoms like fatigue, weight gain, and cold intolerance.
Causes and Risk Factors
While the exact cause of autoimmune diseases is not fully understood, several factors are believed to contribute:
- Genetics: A family history of autoimmune disorder can increase the likelihood of developing one. Certain genes have been linked to a predisposition for autoimmune conditions.
- Environmental Triggers: Factors such as bacterial and parasitic infections, exposure to certain chemicals, or physical trauma may trigger autoimmune responses in genetically susceptible individuals.
- Hormonal Changes: Many autoimmune diseases are more common in women, suggesting that hormonal fluctuations play a role in disease onset.
- Lifestyle Factors: Diet, stress, and smoking have also been implicated in the development and progression of autoimmune disorders.
Symptoms of Autoimmune Diseases
Symptoms can vary widely depending on the type of autoimmune disease and the organs involved. Common symptoms across many autoimmune conditions include:
- Persistent fatigue
- Unexplained weight changes
- Joint pain and swelling
- Skin rashes
- Digestive issues
- Fever
Because these symptoms overlap with many other conditions, autoimmune diseases can be challenging to diagnose.
Diagnosis and Testing
Diagnosing an autoimmune disease typically involves a combination of:
- Medical History: A thorough review of symptoms, family history, and lifestyle factors.
- Physical Examination: Checking for signs of inflammation, joint swelling, and other physical indicators.
- Laboratory Tests: Blood tests can reveal the presence of specific autoantibodies, inflammation markers, or abnormalities in organ function. Common tests include the ANA (antinuclear antibody) test and rheumatoid factor test, as well as nutrient deficiencies. Stool and urine tests can pinpoint bacterial, parasitic, and fungi infections that I always find with autoimmune diseases.
- Imaging Studies: X-rays, MRI, or ultrasound may be used to assess damage to organs and tissues.
Treatment Options
While there is no cure for autoimmune disorders, various treatments can help manage symptoms, improve quality of life, and put symptoms into remission:
- Medications: Anti-inflammatory drugs, immunosuppressants, and disease-modifying antirheumatic drugs (DMARDs) are commonly prescribed to help control the immune response and reduce inflammation. I caution taking these medications due to their side-effects.
- Nutrient Therapy: Nutrient therapy uses therapeutic doses of nutrients (vitamins, minerals and amino acids) and/or botanicals to eliminate infection and create change at the level of DNA (inside the nucleus of the cell). One of the things I love about nutrient therapy is that it does not have the unpleasant side-effects that medications do.
- Lifestyle Changes: Adopting a healthy diet, regular exercise, and stress management techniques can support overall health and well-being.
- Physical Therapy: For diseases affecting the joints or muscles, physical therapy can improve mobility and strength.
- Surgery: In severe cases, surgical interventions may be necessary to repair or replace damaged tissues or organs.
Living with Autoimmune Diseases
Managing an autoimmune disease often requires a multi-faceted approach, including working closely with healthcare providers, staying informed about the condition, and maintaining a supportive network. Regular follow-ups and a proactive approach to managing symptoms can significantly improve quality of life.
Conclusion
Understanding autoimmune diseases is essential for anyone affected by or interested in these complex conditions. By recognizing the symptoms, exploring treatment options, and working with healthcare professionals, individuals can navigate the challenges of autoimmune diseases more effectively. Awareness and education are key to better management and improved outcomes for those living with these chronic conditions.